1/ Definition
What are cruciate ligaments?
The knee has 4 main ligaments ligaments: two lateral ligamentsand two central ligaments that “cross” each other and are called the cruciate ligaments.
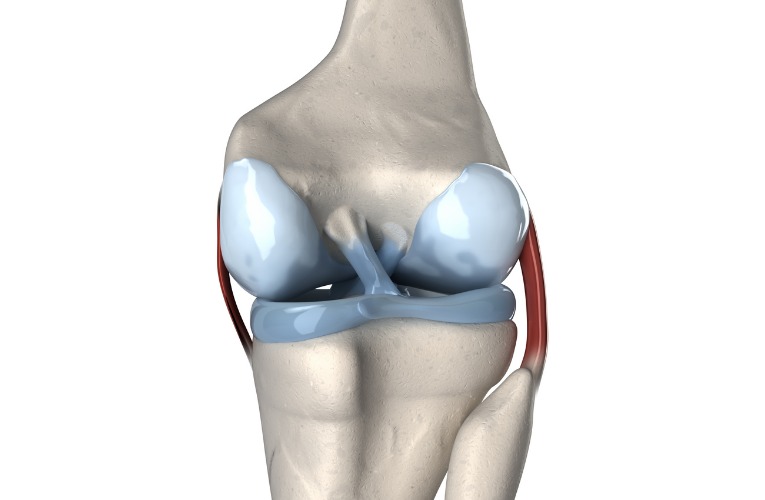
For each knee, we have an anterior cruciate ligament (ACL) and a posterior cruciate ligament (PCL).
In the vast majority of casesit is the anterior cruciate ligament that breaks.
Mechanisms of cruciate ligament rupture
A poorly controlled poorly controlled twisting or excessive extension of the knee can cause a rupture of the cruciate ligament. It is therefore a trauma. It is sometimes accompanied by a cracking sound.
The rupture occurs when the muscles around the knee are not not sufficiently toned and alert and alert at the time of injury.
Here are the three situations causing rupture of the anterior cruciate ligament:
- Valgus, flexion, external rotation
- Varus, flexion, internal rotation
- Sudden extension
It is not uncommon to see breaks on harmless, non-violent falls.
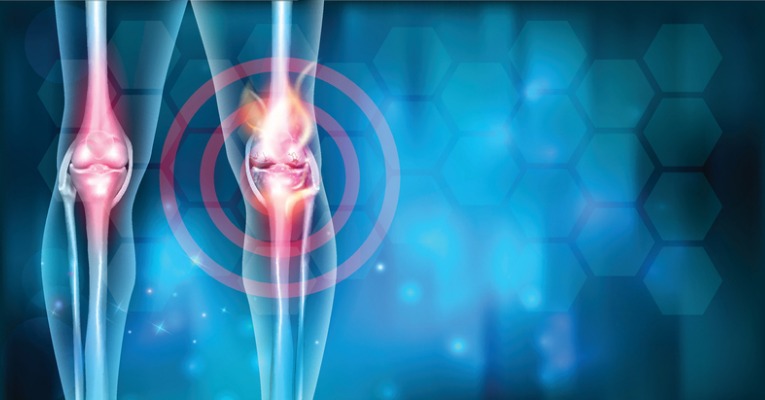
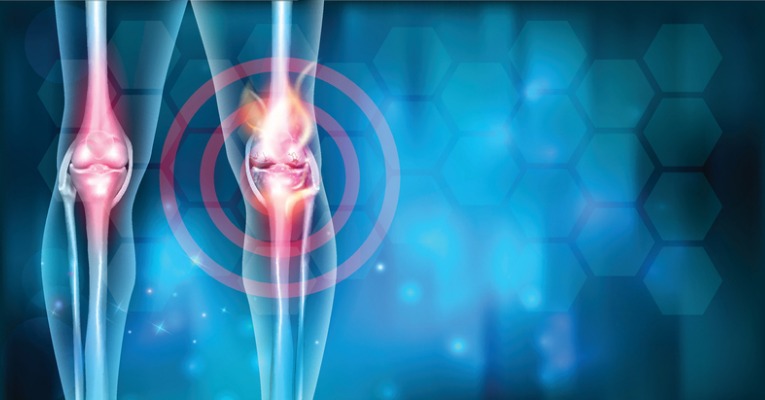
Pain and symptoms
Following this traumatic movement, the knee becomes inflated. This is completely normal, it is a natural physiological process that participates in the healing process.
The pain is often sharp and instantaneous. It usually refers the person for medical advice and additional tests. However, it can sometimes be more moderate, so the doctor is not always consulted.
Most often, we find the classic symptoms of inflammation :
- pain
- swelling (edema)
- redness
- local heat
Once the inflammatory phase is over, other symptoms appear such as a feeling of instability. The knee will appear particularly unstable during sports activities.
If in doubt, consult a competent physician who will be able to guide you to the right course of action.
Special case of partial rupture of the cruciate ligament
The ligament does not always rupture completely. Sometimes only certain fibers are injured. We then talk about partial rupture.
In this case, the ACL is still very fragile and could rupture completely during a future trauma.
A specific rehabilitation is necessary to improve your muscular capacities. The knee is less well stabilized by the ligaments, so it must be better maintained by the muscles!
2/ Explications
What do we see on the X-ray? At the MRI?

The X-ray shows the condition of the bones and cartilage. It allows to know if there is, or not, a associated bone fracture associated.
THE MRI or CT scan are used to observe the state of the ligaments (cruciate ligaments or lateral ligaments) and the menisci.
Once the diagnosis is made, the following questions must be answered:
- What is the degree of knee instability?
- Is there a risk of subluxation during a bad movement?
To answer this question, GNRB testsKT1000 or Telos are more and more used. They accurately measure the degree of knee laxity (laxity of the tibia in relation to the femur) and indicate whether or not surgery is necessary.
Can there be other associated lesions?
1/ The menisci
The internal meniscus is more often affected than the external meniscus. During the operation of the cruciate ligament, the surgeon can then intervene on the damaged meniscus.

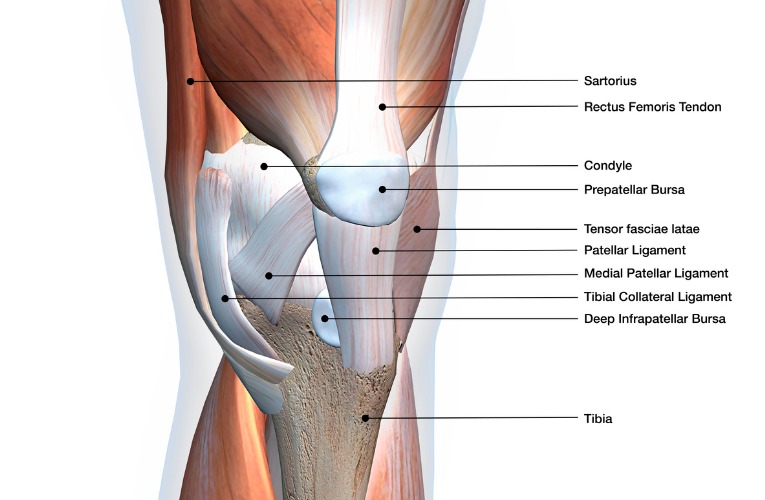
2/ Collateral ligaments
The medial collateral ligament (more frequent) or external can also be affected (sprain). Total ruptures of these ligaments are extremely rare.
3/ The cartilage
During the trauma, the cartilage is sometimes strongly impacted which can cause lesions (cracking, slight cracks…)
What does the operation consist of?
The principle of the surgical operation is to replace the ruptured cruciate ligament with a tendon.
Several surgical techniques can be considered:
DIDT and DT4 are the most common techniques currently used. They use the hamstring tendons.

- The KJ (Kenneth Jones) uses a part of the tendon of the quadriceps musclemuscle, under the patella.
- Techniques using part of the fascia lata (Macintosh, Lemaire).

The operations are, most of the time, performed under arthroscopy. The surgeon makes small openings through which he slides a camera and tools to operate. The scars are discreet and the postoperative care simplified.
The surgical procedure takes less than an hour and is performed under local or general anesthesia. This is a routine operation. The return home is possible the same day or the next day.
After the operation, the knee remains painful for 1 to 2 weeks. You will walk with canes and a splint for 2 to 3 weeks.
What are the long-term risks?
- Without operation
When an unstable knee is heavily used (pivot sports), it risks premature wear (cartilage arthrosis and meniscus degradation).
From time to time, on a false movement, a dislocation (subluxation) can be felt.
In the long term, these instabilities can lead to a general degradation of the cartilage and the periarticular structures.
- After surgery or rehabilitation
After an operation or a functional treatment (rehabilitation) (rehabilitation), the knee should not suffer from instability.
This considerably reduces the risk of premature knee wear in the long term.
Benign postoperative complications
- Slight loss of sensitivity in the skin near the scar:
This insensitivity often worries patients but is not at all troublesome in the long run. This is caused by the section of small nerve endings during the operation. Sensitivity returns most often with time.
- Pain, lack of strength and stiffness of the knee:
These signs are quite common after knee surgery. Time and rehabilitative work will allow a stable and perfectly mobile joint to be found.
- Hematoma (“bruise”) on the back of the knee and/or inside the thigh:
During the operation, bleeding can occur around the joint and down the leg. Depending on their size, it will take one to four weeks for the hematoma to disappear completely.
These complications are quite classic and not serious.
More serious post-operative complications
Some complications require a medical visit in emergency :
- An infection is unfortunately possible during the operation. The surgeon and his team follow very strict hygiene guidelines but there is no such thing as zero risk. During the first few days after surgery, if you have feverthat you are abnormally tired and that you observe a from your scar, do not wait and ask a doctor or call your surgeon.do not wait and ask for a doctor’s advice or call your surgeon urgently.
- A phlebitis can also be a serious complication. It is a blood clot that forms in a vein in the leg. If this clot breaks off and blocks the pulmonary artery (between the heart and lungs), your blood can no longer be recharged with oxygen. This phenomenon is called pulmonary embolism. It is therefore a vital emergency. To avoid any risk of phlebitis, the surgeon will prescribe anticoagulants and compression stockings.
Our advice: Watch carefully for the following clinical signs during the first 10 days
after the operation :
- Signs of phlebitis: painful calf (or unpleasant sensation of tightness), local heat, swelling and stiffness.
- Sign of pulmonary embolism : respiratory discomfort, vague chest pain, increased heart rate, global anxiety.
Fortunately, these cases are rare but should be known before an operation. If in doubt, do not hesitate to call a doctor.
Will my knee be less solid than before?
The surgeon replaces your ruptured ligament with a strong tendon.
Immediately after the operation, this neo-ligament is not innervated (it sends little or no sensory information), and not vascularized (absence of artery-vein blood network). The body will slowly assimilate it as an integral part of the body. It will progressively innervate and vascularize it.
In total, its complete transformation takes nearly 3 years. Its structure is then stronger than the old ligament!
You will regain a strong knee but the full recovery process takes time.
Evolution of the neo-ligament after the operation
Fortunately, you don’t have to wait 3 years to resume your sports activities! The day after the operation, the ligament is still very strong.
This resistance decreases during the first three months after surgery. This is a period during which you must remain vigilant and attentive. A bad fall could affect your transplant.
Once this period has passed, the mechanical strength of the ligament gradually increases. You still need to undergo serious rehabilitation to return to sport in good conditions.
The ligament is considered sufficiently strong one year after the operation to resume competitive sports.
In the long term, if you have followed your rehabilitation rigorously, you will no longer think about your knee and you will be able to practice your sports activities as before.
3/ Durée du traitement
What happens after the operation? The different stages of your rehabilitation
- You will probably be able to go home the day same day of the operation. This device, called “outpatient surgery”, is most often practiced today. Make sure that someone close to you can accompany you back home.
- During the first week after the operation, the knee is often painful. The surgeon will prescribe anti-inflammatory or analgesic drugs to calm the pain. Generally, this will subside after one week after the operation.
- A bandage will cover the scar to protect it. A nurse will take care of the scar and the dressing.
- To avoid any risk of phlebitisyou must wear compression stockings for 1 to 2 weeks.
- You will use crutches to move because the knee will not be strong enough to support the weight of the body. During the first days, two crutches will be necessary. Soon you will be able to take only one.

- You will also wear a splint to maintain the knee. You will be forced to wear it every time you walk. You can however remove it regularly during the day to leave the knee free from time to time.

- Rehabilitation begins from the first days after the operation. You will gradually regain some flexibility in your knee, but it will still remain relatively weak. You will not be able to drive a car for at least 1 month after the operation.
- From the 3th weekyou can remove the splint even while walking. At first, you will only take a few steps at home. Afterwards, you will remove the splint even to go out walking for longer distances (usually not before 3 weeks – one month after surgery).
- One month after the operationYou will be able to walk more or less normally without a cane or splint. On the other hand, going up and down the stairs will always be an ordeal for you.
- Leg swimming (no breaststroke at first) is generally recommended from the 3rd month. Similarly, the use of fins is not recommended at the beginning of rehabilitation because it puts a lot of strain on the knee.
- You can run from 4th month after the operation.

- More intense sports such as soccer, tennis, basketball, handball, skiing etc. can be resumed very gradually from 6-8 months after the operation. You will then wear a knee brace for several weeks and remove it afterwards. Contact with the opponent is not recommended before the 9thème month. You will resume with light workouts at first.
- It is advisable not to resume competitive sports (contact, high intensity…) until about one year after the operation.
When should I have surgery?

There is no no emergency to operate on a cruciate ligament. It is possible to wait several months or years. Professional athletes undergo surgery without delay because they want to return to competition as soon as possible. However, if you are not a high level athlete, it is better to wait for the knee to deflate and that the inflammation decreases.
Going into surgery with a swollen, painful knee that lacks mobility and strength makes the post-operative aftermath more difficult.
What are the factors that lead to an operation or not?
- Sports practiced
If you practice a pivot sport (skiing, tennis, soccer, basketball, handball, etc.), the operation is highly recommended.
If you practice a sport such as cycling or swimming, your knee will be less stressed in rotation. The risk of instability is therefore lower. A functional treatment (rehabilitation without surgery) may be sufficient.
- The importance of laxity
In some people, a cruciate ligament rupture causes very little instability because the knee remains well supported by other anatomical structures. For them, the operation can be questioned.
The GNRB test test allows to quantify this instability.
- The age
An unstable knee will wear out more quickly over the years. This is why the operation is strongly recommended for people under 30 years of age. After the age of 50, the decision to operate is less systematic.
- Associated lesions
If the meniscus is injured in addition to the cruciate ligament rupture, then surgery is more strongly recommended. Depending on the type of lesion, it may be worthwhile not to wait too long before operating.
In summary, each of these four parameters must be taken into account when deciding whether or not to undergo surgery. Don’t hesitate to consult several specialists to make a decision. Once again, no rush !
Cruciate ligament rupture: what should be done?
- If you do not wish to have surgeryIn order to stabilize the joint, you must do serious rehabilitation to stabilize the joint through the muscular system. Strengthening and proprioception exercises will be given. Re-education helps to overcome ligament instability.
- If you are planning to have surgery, you should also practice a pre-operative rehabilitation to place the knee in optimal conditions for recovery. The post-operative aftermath will then be easier. The goal of the treatment is to restore a painless, flexible, perfectly mobile and as stable as possible joint before the operation. Hip, thigh and calf muscles will be strengthened.
Articles liés
1/ Definition
What are cruciate ligaments?
The knee has 4 main ligaments ligaments: two lateral ligamentsand two central ligaments that “cross” each other and are called the cruciate ligaments.
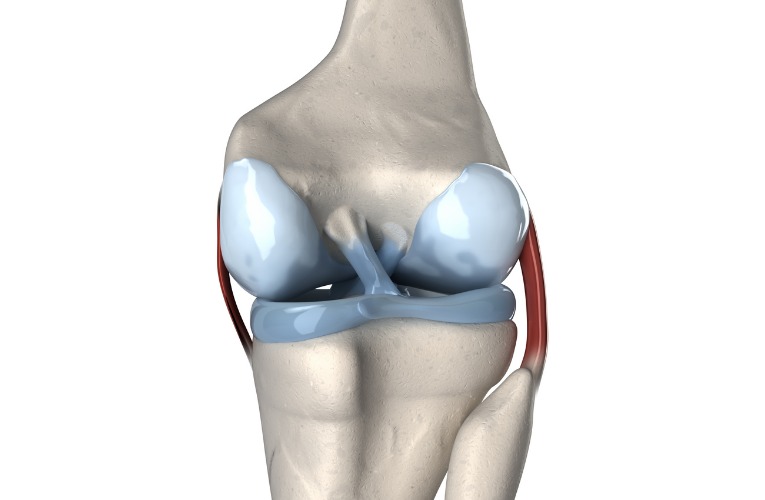
For each knee, we have an anterior cruciate ligament (ACL) and a posterior cruciate ligament (PCL).
In the vast majority of casesit is the anterior cruciate ligament that breaks.
Mechanisms of cruciate ligament rupture
A poorly controlled poorly controlled twisting or excessive extension of the knee can cause a rupture of the cruciate ligament. It is therefore a trauma. It is sometimes accompanied by a cracking sound.
The rupture occurs when the muscles around the knee are not not sufficiently toned and alert and alert at the time of injury.
Here are the three situations causing rupture of the anterior cruciate ligament:
- Valgus, flexion, external rotation
- Varus, flexion, internal rotation
- Sudden extension
It is not uncommon to see breaks on harmless, non-violent falls.
Pain and symptoms
Following this traumatic movement, the knee becomes inflated. This is completely normal, it is a natural physiological process that participates in the healing process.
The pain is often sharp and instantaneous. It usually refers the person for medical advice and additional tests. However, it can sometimes be more moderate, so the doctor is not always consulted.
Most often, we find the classic symptoms of inflammation :
- pain
- swelling (edema)
- redness
- local heat
Once the inflammatory phase is over, other symptoms appear such as a feeling of instability. The knee will appear particularly unstable during sports activities.
If in doubt, consult a competent physician who will be able to guide you to the right course of action.
Special case of partial rupture of the cruciate ligament
The ligament does not always rupture completely. Sometimes only certain fibers are injured. We then talk about partial rupture.
In this case, the ACL is still very fragile and could rupture completely during a future trauma.
A specific rehabilitation is necessary to improve your muscular capacities. The knee is less well stabilized by the ligaments, so it must be better maintained by the muscles!
2/ Explications
What do we see on the X-ray? At the MRI?

The X-ray shows the condition of the bones and cartilage. It allows to know if there is, or not, a associated bone fracture associated.
THE MRI or CT scan are used to observe the state of the ligaments (cruciate ligaments or lateral ligaments) and the menisci.
Once the diagnosis is made, the following questions must be answered:
- What is the degree of knee instability?
- Is there a risk of subluxation during a bad movement?
To answer this question, GNRB testsKT1000 or Telos are more and more used. They accurately measure the degree of knee laxity (laxity of the tibia in relation to the femur) and indicate whether or not surgery is necessary.
Can there be other associated lesions?
1/ The menisci
The internal meniscus is more often affected than the external meniscus. During the operation of the cruciate ligament, the surgeon can then intervene on the damaged meniscus.

2/ Collateral ligaments
The medial collateral ligament (more frequent) or external can also be affected (sprain). Total ruptures of these ligaments are extremely rare.
3/ The cartilage
During the trauma, the cartilage is sometimes strongly impacted which can cause lesions (cracking, slight cracks…)
What does the operation consist of?
The principle of the surgical operation is to replace the ruptured cruciate ligament with a tendon.
Several surgical techniques can be considered:
DIDT and DT4 are the most common techniques currently used. They use the hamstring tendons.

- The KJ (Kenneth Jones) uses a part of the tendon of the quadriceps musclemuscle, under the patella.
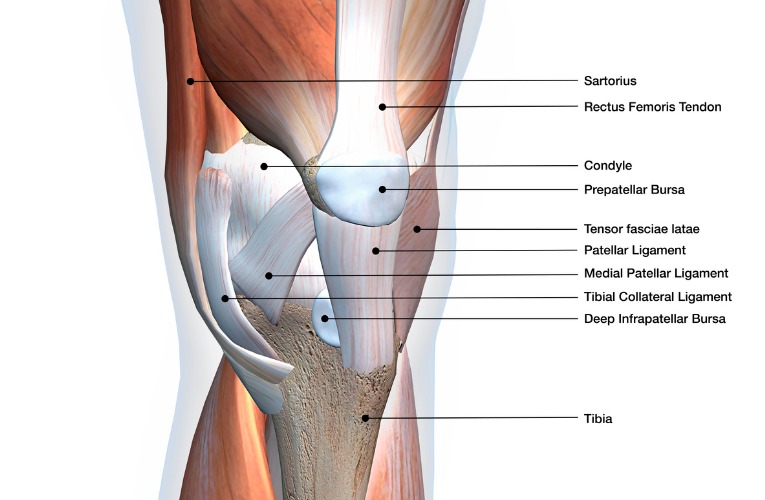
- Techniques using part of the fascia lata (Macintosh, Lemaire).

The operations are, most of the time, performed under arthroscopy. The surgeon makes small openings through which he slides a camera and tools to operate. The scars are discreet and the postoperative care simplified.
The surgical procedure takes less than an hour and is performed under local or general anesthesia. This is a routine operation. The return home is possible the same day or the next day.
After the operation, the knee remains painful for 1 to 2 weeks. You will walk with canes and a splint for 2 to 3 weeks.
What are the long-term risks?
- Without operation
When an unstable knee is heavily used (pivot sports), it risks premature wear (cartilage arthrosis and meniscus degradation).
From time to time, on a false movement, a dislocation (subluxation) can be felt.
In the long term, these instabilities can lead to a general degradation of the cartilage and the periarticular structures.
- After surgery or rehabilitation
After an operation or a functional treatment (rehabilitation) (rehabilitation), the knee should not suffer from instability.
This considerably reduces the risk of premature knee wear in the long term.
Benign postoperative complications
- Slight loss of sensitivity in the skin near the scar:
This insensitivity often worries patients but is not at all troublesome in the long run. This is caused by the section of small nerve endings during the operation. Sensitivity returns most often with time.
- Pain, lack of strength and stiffness of the knee:
These signs are quite common after knee surgery. Time and rehabilitative work will allow a stable and perfectly mobile joint to be found.
- Hematoma (“bruise”) on the back of the knee and/or inside the thigh:
During the operation, bleeding can occur around the joint and down the leg. Depending on their size, it will take one to four weeks for the hematoma to disappear completely.
These complications are quite classic and not serious.
More serious post-operative complications
Some complications require a medical visit in emergency :
- An infection is unfortunately possible during the operation. The surgeon and his team follow very strict hygiene guidelines but there is no such thing as zero risk. During the first few days after surgery, if you have feverthat you are abnormally tired and that you observe a from your scar, do not wait and ask a doctor or call your surgeon.do not wait and ask for a doctor’s advice or call your surgeon urgently.
- A phlebitis can also be a serious complication. It is a blood clot that forms in a vein in the leg. If this clot breaks off and blocks the pulmonary artery (between the heart and lungs), your blood can no longer be recharged with oxygen. This phenomenon is called pulmonary embolism. It is therefore a vital emergency. To avoid any risk of phlebitis, the surgeon will prescribe anticoagulants and compression stockings.
Our advice: Watch carefully for the following clinical signs during the first 10 days
after the operation :
- Signs of phlebitis: painful calf (or unpleasant sensation of tightness), local heat, swelling and stiffness.
- Sign of pulmonary embolism : respiratory discomfort, vague chest pain, increased heart rate, global anxiety.
Fortunately, these cases are rare but should be known before an operation. If in doubt, do not hesitate to call a doctor.
Will my knee be less solid than before?
The surgeon replaces your ruptured ligament with a strong tendon.
Immediately after the operation, this neo-ligament is not innervated (it sends little or no sensory information), and not vascularized (absence of artery-vein blood network). The body will slowly assimilate it as an integral part of the body. It will progressively innervate and vascularize it.
In total, its complete transformation takes nearly 3 years. Its structure is then stronger than the old ligament!
You will regain a strong knee but the full recovery process takes time.
Evolution of the neo-ligament after the operation
Fortunately, you don’t have to wait 3 years to resume your sports activities! The day after the operation, the ligament is still very strong.
This resistance decreases during the first three months after surgery. This is a period during which you must remain vigilant and attentive. A bad fall could affect your transplant.
Once this period has passed, the mechanical strength of the ligament gradually increases. You still need to undergo serious rehabilitation to return to sport in good conditions.
The ligament is considered sufficiently strong one year after the operation to resume competitive sports.
In the long term, if you have followed your rehabilitation rigorously, you will no longer think about your knee and you will be able to practice your sports activities as before.
3/ Durée du traitement
What happens after the operation? The different stages of your rehabilitation
- You will probably be able to go home the day same day of the operation. This device, called “outpatient surgery”, is most often practiced today. Make sure that someone close to you can accompany you back home.
- During the first week after the operation, the knee is often painful. The surgeon will prescribe anti-inflammatory or analgesic drugs to calm the pain. Generally, this will subside after one week after the operation.
- A bandage will cover the scar to protect it. A nurse will take care of the scar and the dressing.
- To avoid any risk of phlebitisyou must wear compression stockings for 1 to 2 weeks.
- You will use crutches to move because the knee will not be strong enough to support the weight of the body. During the first days, two crutches will be necessary. Soon you will be able to take only one.

- You will also wear a splint to maintain the knee. You will be forced to wear it every time you walk. You can however remove it regularly during the day to leave the knee free from time to time.

- Rehabilitation begins from the first days after the operation. You will gradually regain some flexibility in your knee, but it will still remain relatively weak. You will not be able to drive a car for at least 1 month after the operation.
- From the 3th weekyou can remove the splint even while walking. At first, you will only take a few steps at home. Afterwards, you will remove the splint even to go out walking for longer distances (usually not before 3 weeks – one month after surgery).
- One month after the operationYou will be able to walk more or less normally without a cane or splint. On the other hand, going up and down the stairs will always be an ordeal for you.
- Leg swimming (no breaststroke at first) is generally recommended from the 3rd month. Similarly, the use of fins is not recommended at the beginning of rehabilitation because it puts a lot of strain on the knee.
- You can run from 4th month after the operation.

- More intense sports such as soccer, tennis, basketball, handball, skiing etc. can be resumed very gradually from 6-8 months after the operation. You will then wear a knee brace for several weeks and remove it afterwards. Contact with the opponent is not recommended before the 9thème month. You will resume with light workouts at first.
- It is advisable not to resume competitive sports (contact, high intensity…) until about one year after the operation.
When should I have surgery?

There is no no emergency to operate on a cruciate ligament. It is possible to wait several months or years. Professional athletes undergo surgery without delay because they want to return to competition as soon as possible. However, if you are not a high level athlete, it is better to wait for the knee to deflate and that the inflammation decreases.
Going into surgery with a swollen, painful knee that lacks mobility and strength makes the post-operative aftermath more difficult.
What are the factors that lead to an operation or not?
- Sports practiced
If you practice a pivot sport (skiing, tennis, soccer, basketball, handball, etc.), the operation is highly recommended.
If you practice a sport such as cycling or swimming, your knee will be less stressed in rotation. The risk of instability is therefore lower. A functional treatment (rehabilitation without surgery) may be sufficient.
- The importance of laxity
In some people, a cruciate ligament rupture causes very little instability because the knee remains well supported by other anatomical structures. For them, the operation can be questioned.
The GNRB test test allows to quantify this instability.
- The age
An unstable knee will wear out more quickly over the years. This is why the operation is strongly recommended for people under 30 years of age. After the age of 50, the decision to operate is less systematic.
- Associated lesions
If the meniscus is injured in addition to the cruciate ligament rupture, then surgery is more strongly recommended. Depending on the type of lesion, it may be worthwhile not to wait too long before operating.
In summary, each of these four parameters must be taken into account when deciding whether or not to undergo surgery. Don’t hesitate to consult several specialists to make a decision. Once again, no rush !
Cruciate ligament rupture: what should be done?
- If you do not wish to have surgeryIn order to stabilize the joint, you must do serious rehabilitation to stabilize the joint through the muscular system. Strengthening and proprioception exercises will be given. Re-education helps to overcome ligament instability.
- If you are planning to have surgery, you should also practice a pre-operative rehabilitation to place the knee in optimal conditions for recovery. The post-operative aftermath will then be easier. The goal of the treatment is to restore a painless, flexible, perfectly mobile and as stable as possible joint before the operation. Hip, thigh and calf muscles will be strengthened.



